Liver failure decision making; getting it right first time with metabolic profiling
Liver disease is the fifth commonest cause of death in the developed world. The global burden of liver cirrhosis is rising owing to an increased prevalence of alcohol and non-alcoholic-liver disease. Standardised mortality in the UK has risen by 400% from 1970 and the incidence of patients with cirrhosis in UK intensive care units (ICUs) has tripled since 1998.
Two forms of liver failure are possible; A) Acute liver failure (ALF), where hepatic cell death occurs on the background of normal liver function, and B) Acute-On-Chronic Liver Failure (ACLF), when patients with cirrhosis progress to multi-organ failure. Both forms of liver failure are associated with metabolic disarray, immune dysfunction, high short-term mortality and significant healthcare costs. Decisions regarding suitability for life-saving therapies (e.g. liver transplantation (LT)) or ICU admission are assisted by prognostic scoring models. However, they lack precision, disadvantaging access to transplantation or ICU care resulting in thousands of preventable deaths each year. For those who are likely to survive spontaneously then avoiding unnecessary transplantation prevents the need for lifelong immunosuppressant medication and frees a donor liver for another patient.
Can a clinically useful prognostic blood test be developed using lipidomics?
The NPC applied their unique multi-platform metabolic phenotyping (untargeted 1H NMR spectroscopy and ultra-performance liquid chromatography coupled with mass spectrometry (UPLC-MS)) of plasma in patients ACLF. This led to a robust predictive model of 90-day survival, based on a panel of discriminatory lipids (mainly phosphocholines (PCs) and lysophosphatidylcholines (LPCs)). This was substantially superior to existing clinical scoring systems that predict survival. Further validation experiments using lipid-optimised profiling of serum have confirmed that lipids are powerful prognostic biomarkers with a consistent accuracy of over 95% and definitive metabolite identification is needed.
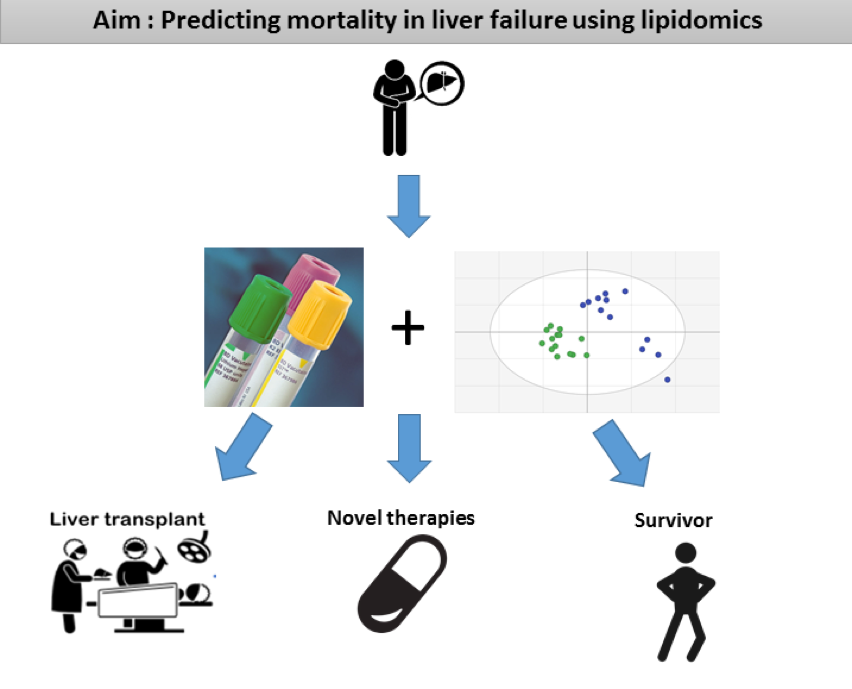
Further work will include targeted method optimisation for the most useful metabolites and development of a fully-quantified method more suitable for a healthcare setting, before these findings can be applied to clinical decision-making are required.
The next stage of this project aims to make a step change in addressing this knowledge gap – by finding the most effective prognostic panels employing the robust platform developed by National Phenome Centre. A multicentre prospective longitudinal cohort study metabolically profiling patients with cirrhosis and acute liver failure to radically improve prognostication at key decision points.
Metabolome to Product
A blood test suitable for clinical laboratories based on quantitative lipid analysis for the accurate prediction of hospital mortality.
Acknowledgements: Infrastructure support was provided by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC)
Return to Case Studies