Urinary Metabolic Phenotyping of Women with Lower Urinary Tract Symptoms (LUTS)
Lower urinary tract symptoms (LUTS), including urinary incontinence, urgency and nocturia are highly prevalent across all ages, and more than half of women worldwide experience at least one. The condition affects quality of life, daily activities and it has significant effects on physical and mental health. In addition, it means a significant economic burden, with direct costs estimated to be $11 billion/year in the United States alone for overactive bladder (OAB), the most prevalent LUTS.
Objective diagnostic criteria are lacking for the majority of LUTS and there is a concern that the current algorithms fail to account for the underlying pathogenesis of the symptoms. Those that exist, such as the urodynamic testing, are invasive and lack prognostic significance. In addition, treatment strategies for LUTS are often hindered by side effects and poor patient compliance. The identification of novel, non-invasive biomarkers would provide substantial clinical benefit in helping to direct and tailor treatments.
Can Metabolic Profiling be used for the Stratification of LUTS patients and help with the Designing of Tailored Treatment Strategies?
In this study 214 women were recruited and their urine samples were analysed by 1H nuclear magnetic resonance spectroscopy (NMR) to obtain their metabolic profiles. 176 women were suffering LUTS and the rest were healthy volunteers whose samples were used as controls.
Multivariate statistical analysis was used to determine whether perturbations in the urinary metabolome can be associated with LUTS and thus provide unique metabolic signatures useful for diagnostic and stratification purposes.
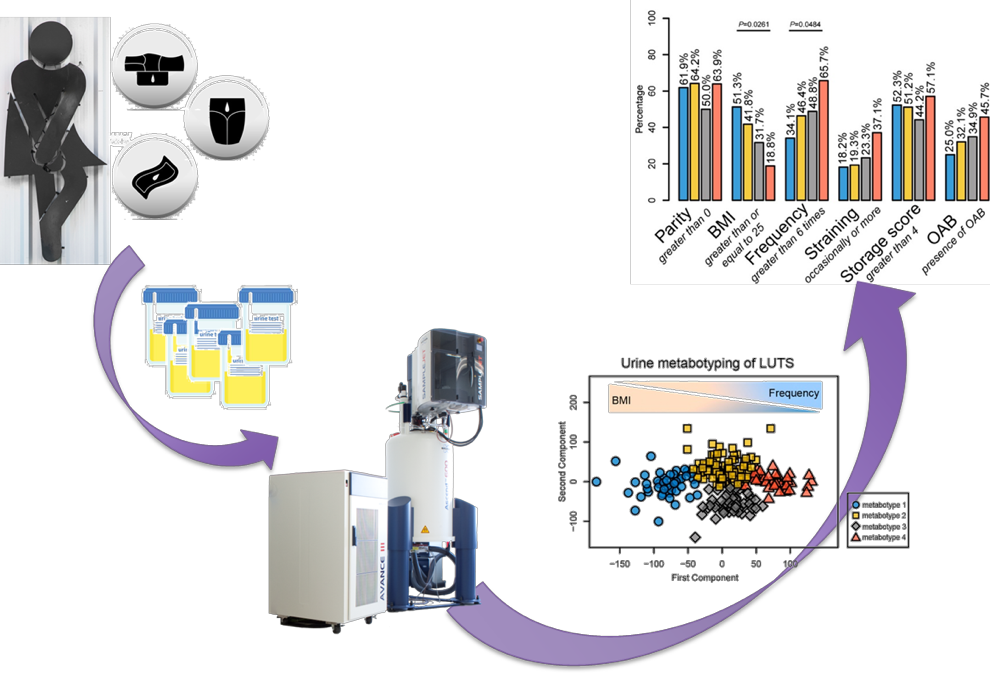
1H NMR analysis of urine from women showing different types of LUTS were associated with different metabotypes which are related with clinical features. The two main differentiating factors of the urinary metabotypes observed are BMI and frequency. However, there were other factors such as parity, straining, storage score, OAB which also contribute to the different LUTS metabotypes. The biomarkers associated with the two main metabotypes are hippurate, phenylacetylglutamine, glucose, threonine, creatinine, phosphocreatinine, trimethylamine-N-oxide, alanine, 2-ketoisovalerate, creatine, acetate, lactate, isoleucine, 2-hydroxyisobutyrate and tyrosine.
This study indicates that the multi-aetiological pathogenesis of individual LUTS is reflected in a highly variable urinary metabolome. However this urinary metabolome can be associated with clinical features providing an objective description of a very heterogeneous syndrome. Future metabolic profiling studies of LUTS may benefit from detailed assessment of stratified demographic cohorts (e.g., treatment responder and non-responder phenotypes indicative of underlying aetiology) and longitudinal analyses of patients receiving interventions.
Metabolome to Product
A urine test based on changes in metabolite concentrations for the identification of differences in underlying aetiology. This will permit stratification of patient populations and the design of more personalized treatment strategies which will improve quality of life for patients and decrease costs for governments.
Acknowledgements: Infrastructure support was provided by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC)
Return to Case Studies