Inflammatory Bowel Disease and Effect of other Comorbidities
Inflammatory Bowel Disease (IBD) is a term used to describe different idiopathic disease of the gastrointestinal tract. It normally involves severe diarrhoea, abdominal pain, fatigue and weight loss. There is currently no cure for IBD, all the treatments aim to palliate symptoms, however 1 out of 5 patients don’t improve with medication. Patients with IBD have also an increased risk of developing bowel cancer.
IBD is a very heterogenous condition with a variety of symptoms and phenotypes. The phenotypes are known to have a genetic component but there is an important contribution of the gut microbiome, which is unique in every individual and affected by diet and lifestyle and supports the concept of gut dysbiosis in IBD pathogenesis. Unfortunately patients with IBD very often suffer from other conditions such as diabetes, asthma or cardiovascular diseases.
Understanding the relationship between genetics, gut microbiota, diet, life style and other comorbidities is essential to improve patient stratification, disease management and adequate treatment design.
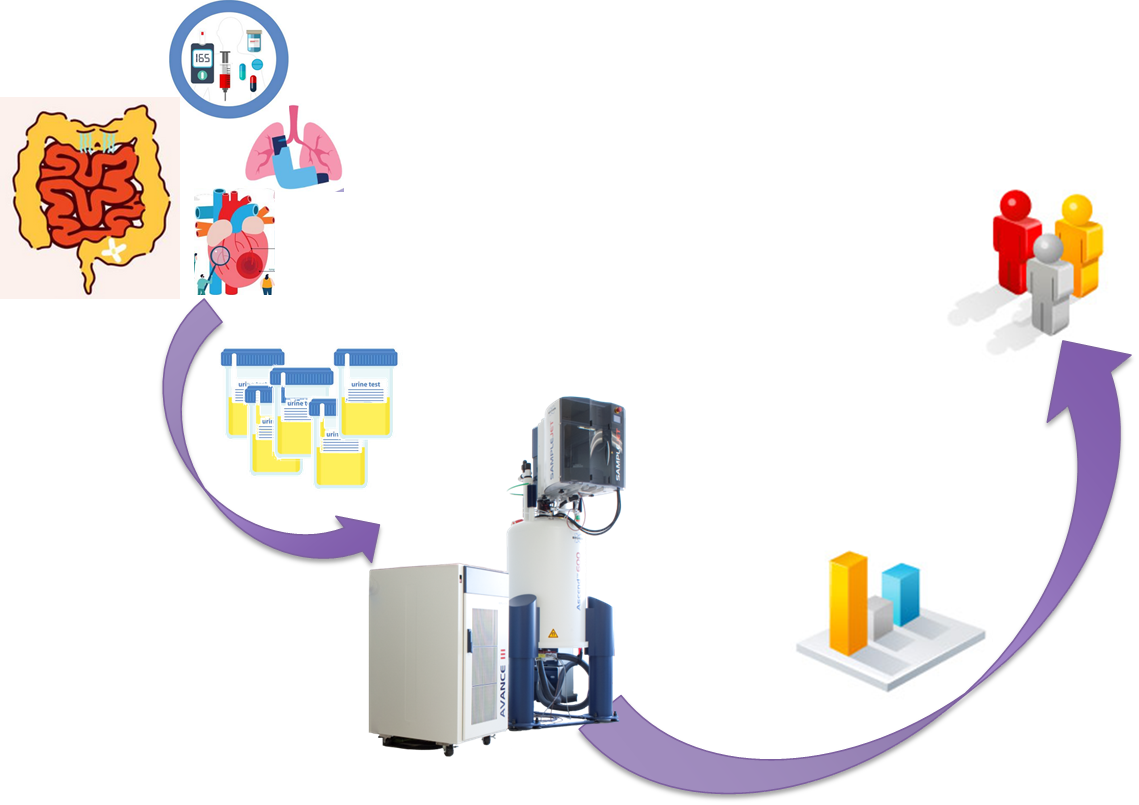
Are the urinary phenotypes of patients with IBD affected by other diseases?
Urine samples from 51 IBD patients with at least one significant comorbidity (including diabetes mellitus, asthma and ischaemic heart disease), 46 patients with IBD alone, and 54 healthy controls were collected and analysed using 1H NMR spectroscopy and multivariate statistics.
Univariate analysis showed that hippurate excretion was significantly lower in patients with IBD with and without comorbidities compared to healthy controls confirming gut microbiome metabolic dysfunction. In addition, trimethylamine (TMA) levels were relatively increased in patients with only IBD and those with other comorbidities compared to healthy controls, although trimethylamine-N-oxide (TMAO) levels showed no significant difference due to IBD or comorbid status. The relative increase in TMA has not been previously reported in humans, but correlates with a study that shows increasing TMA with progression of IBD in the IL10 knock-out mouse model.
The urinary metabolic profiles studied showed clear differences between patients suffering IBD compared to healthy controls, however, the differences between the metabolic phenotypes of patients suffering only IBD or IBD with other comorbidities were more subtle, and mainly dominated by the IBD fingerprint.
An in-depth multivariate statistical modelling of this dataset is required to elucidate metabolic phenotypes associated with complex comorbidities in IBD
Metabolome to Product
Establish a panel of metabolites related not only with IBD but with the different comorbidities which more commonly affect IBD patients to help manage IBD patients and tailor treatments.
Return to Case Studies